Digital Pathology is a new data source to transform medicine
Medscape – Oct 15, 2014.
This was the hook line of a 2014 article in Medscape we stumbled across the other day. Ten years later, it’s time to take stock and to check if the impact of digital pathology was indeed transformational. (Spoiler alert: They were right!)
Here’s our ultimate guide:
10 Things You Should Know about Digital Pathology –
and things to consider for the bright digital future ahead
| 1 | The Covid pandemic helped: The possibility to work from home has become one of the key drivers for digital pathology (and telepathology). |
| 2 | And so has the lack of new pathologists (“workforce crisis”). A new hire might prefer working in a (digital) practice that supports occasionally working from home over a traditional (analog) practice. |
| 3 | Finally, in 2022 and 2023 a multitude of AIs received CE-IVDR clearance and can be used in the routine. |
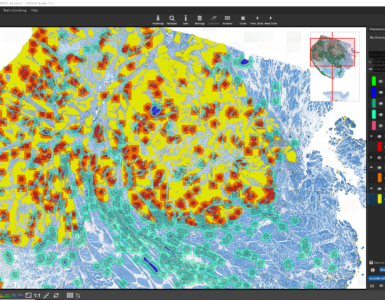
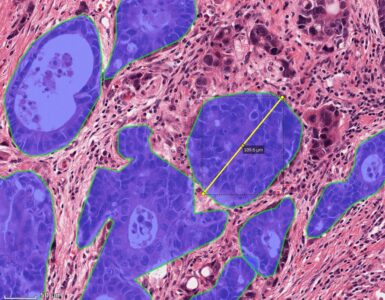
| 4 | Digital pathology is often referred to as the “3rd revolution” in pathology, following the introduction of immuno-histochemistry (IHC) as the 1st revolution and molecular pathology as the 2nd revolution. |
| 5 | Digital pathology produces gigabytes of data – each day. A single scan takes between 1-3 GB, sometimes even more. Most labs that decide to go fully digital and scan each and every glass slide use a “rolling archive” that starts overwriting scans after 1-3 months, ensuring the archive does not grow endlessly. Slides can be tagged to keep them forever, e.g., when they are medically interesting or may become relevant from a legal perspective. Some labs store slides “on-prem” in a local storage (higher up- front costs and hardware has to be replaced during its lifetime), others in the cloud (continuous metered fees per terabyte). |
| 6 | Main reasons for NOT going digital are: 1. The workflow is changed entirely: Technical assistants constantly feed slides into the scanner. Scanners can work over night. Pathologists open and review case on their computer. Scanners represent an additional processing step and with it an additional point of failure. Scans can sometimes be out-of-focus, and slides may break, which can even jam the scanner. 2. The costs: Approximately one scanner per pathologist is required. Additionally, an Image Management System (IMS, aka Histo-PACS) has to be introduced and it needs to be compatible with the LIS to ensure the same case is opened in both systems. LIS and IMS are typically open side-by-side on two monitors. Some labs use this occasion to switch their LIS as well. Aside from the up-front costs, the archive for storing the scans produces high costs over time. The business case is not clear. The image quality: Some pathologists prefer the quality of their analog microscope over that of a scanner. 3. The image quality: Some pathologists prefer the quality of their analog microscope over that of a scanner. |
| 7 | There is still no standard imaging-format. While in radiology, it is crystal clear that images are stored in the DICOM format, in pathology most vendors use their own proprietary formats. Sure, a DICOM-WSI format also exists and is gaining traction. Maybe one day it will replace the proprietary formats. Let’s check back in another 10 years. |
| 8 | The little brother of digital pathology is to introduce computer-readable slide labels that contain barcodes or QR-codes, coding the case ID and type of stain. |
| 9 | Digital pathology is a pre-requirement for Computational Pathology, i.e., going digital unlocks the door into the world of AI. AIs can be integrated into the IMS to automatically conduct analyses after scanning – before a pathologist even opens the case. For instance, introducing an AI that detects metastases in lymph node sections allows sorting the slides of a case by decreasing tumor presence probabilities; heatmaps can guide the pathologist’s gaze to a particular area in a slide. This can save time, or it can be regarded as a second look and decrease the risk that a (micro) metastasis is missed. Other types of AIs include Gleason Grading for prostate cancer, Ki67 or PD-L1 scoring for breast or NSCLC. Many more AIs are available and new ones are becoming available at a rapidly growing pace. |
| 10 | Currently, in many countries, labs do not get reimbursed for the additional cost for scanning or AI analysis. An exception is the US, where scanning is reimbursed. |




Add comment